Living with diabetes in South Africa presents unique challenges, but what many don’t realize is the profound impact it can have on oral health.
As someone who has navigated the complexities of managing diabetes firsthand, I’ve come to understand the critical connection between blood sugar levels and oral well-being.
In this guide, we’ll explore the intricate relationship between diabetes and oral health, the complications that can arise, and actionable tips to help diabetics maintain a healthy smile.
Quick Summary
- Diabetes affects more than just blood sugar — it has a direct impact on oral health.
- Common oral complications include gum disease, dry mouth, fungal infections, poor healing, and cavities.
- High blood sugar feeds bacteria, weakens immunity, and increases inflammation, all of which harm the gums.
- Oral health management is essential because gum disease can worsen blood sugar control, creating a two-way relationship.
- Practical tips: brush twice daily, floss daily, stay hydrated, avoid sugary foods/drinks, and visit the dentist regularly.
Understanding Diabetes
Diabetes is a chronic condition that affects how your body regulates blood sugar. Here’s a quick breakdown of the key points:
How Diabetes Affects Your Body
- Blood Sugar and Insulin: Your body breaks down food into glucose (sugar), which is then used for energy. Insulin, a hormone produced by the pancreas, acts like a key, allowing glucose to enter cells.
- The Problem: In diabetes, either your body doesn’t produce enough insulin (type 1 diabetes), or the cells resist insulin’s effects (type 2 diabetes). This results in excess sugar buildup in the bloodstream.
- Long-Term Effects: Over time, high blood sugar levels can damage various organs, including nerves, eyes, kidneys, and the heart.
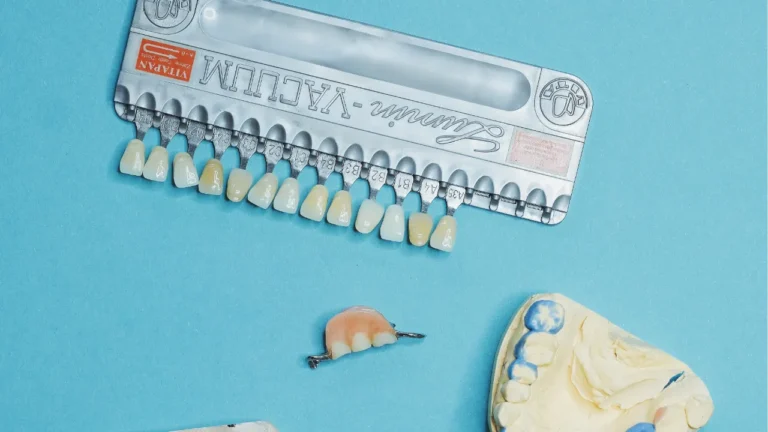
Oral Health Complications Associated with Diabetes
Diabetes can significantly impact your oral health, increasing your risk for various complications. Here’s a breakdown of the common ones:
- Gum Disease: People with diabetes are more prone to gum disease, including gingivitis (inflammation) and periodontitis (severe gum infection that damages bone).
- Dry Mouth: Unmanaged diabetes can decrease saliva production, leading to dry mouth. Saliva plays a vital role in washing away food particles, preventing cavities, and maintaining a healthy mouth environment.
- Fungal Infections: Thrush, a fungal infection, is more common in people with diabetes. It causes white patches to form on the tongue and inner cheeks.
- Poor Healing: Diabetes can slow down wound healing after dental procedures, increasing the risk of infection.
- Increased Cavities: Some studies suggest that people with uncontrolled diabetes may be at higher risk for cavities.
Mechanisms Behind the Link
The link between diabetes and oral health complications is a two-way street, with several mechanisms at play:
High Blood Sugar’s Impact on Oral Health:
- Fueling Bacterial Growth: Uncontrolled diabetes means high blood sugar levels in your saliva. This sugary environment acts like a buffet for bacteria in your mouth, promoting their growth and plaque buildup.
- Weakened Immune System: Diabetes can hinder your immune system’s ability to fight off infections, including those in the gums. This makes it harder to control gum disease once it starts.
- Inflammatory Response: Chronically high blood sugar contributes to inflammation throughout the body, including the gums. This inflammation further damages gum tissue and bone, worsening gum disease.
Importance of Oral Health Management for Diabetics
For people with diabetes, managing oral health becomes even more critical than for those without. Here’s why:
- Increased Risk of Gum Disease: Diabetes creates a double whammy for your gums. High blood sugar feeds bacteria that cause plaque buildup, and diabetes weakens the immune system’s ability to fight gum infections. This significantly increases the risk of gingivitis and periodontitis, which can damage gum tissue and bone, potentially leading to tooth loss.
- Blood Sugar Control: There’s a two-way street between gum disease and diabetes. Uncontrolled gum disease can worsen blood sugar control, making it harder to manage diabetes. Conversely, good oral hygiene habits and regular dental care can help improve blood sugar control.
- Complications: Unmanaged gum disease in diabetics can increase the risk of other health complications, such as heart disease and stroke.
- Comfort and Well-being: Oral health problems like gum disease and cavities can be painful and make eating difficult. Maintaining good oral health ensures better overall comfort and well-being for diabetics.
Tips for Diabetics to Maintain Oral Health
Here are some key tips for diabetics to maintain good oral health:
- Brushing: Brush your teeth at least twice a day for two minutes each time, using a soft-bristled toothbrush and fluoride toothpaste.
- Flossing: Floss once a day to remove plaque and food particles from between your teeth.
- Diet: Limit sugary foods and drinks, which can contribute to plaque buildup and cavities.
- Dry Mouth: If you experience dry mouth, drink plenty of water throughout the day and consider sugar-free gum or lozenges to stimulate saliva production.
- Regular Dental Checkups: See your dentist for checkups and cleanings at least twice a year, or more often if recommended by your dentist. Early detection and treatment of oral health problems are crucial for diabetics.
Conclusion
As someone who understands the daily struggles of managing diabetes, I can attest to the importance of prioritizing oral health.
By acknowledging the link between diabetes and oral complications and taking proactive steps to address it, we can pave the way for healthier smiles and happier lives.
Let’s start the conversation and empower each other to thrive, both physically and orally.